This is part of our series on hidden or stigmatised health conditions in men. Read the other articles in the series here.
Klinefelter’s syndrome is a genetic disorder that affects approximately one in 450 males. Each cell in the human body has 23 pairs of chromosomes. The sex chromosomes in a female are XX, and XY in men. Typically, men have 46 chromosomes with an arrangement of 46XY, while those with Klinefelter’s syndrome have a 47XXY arrangement.

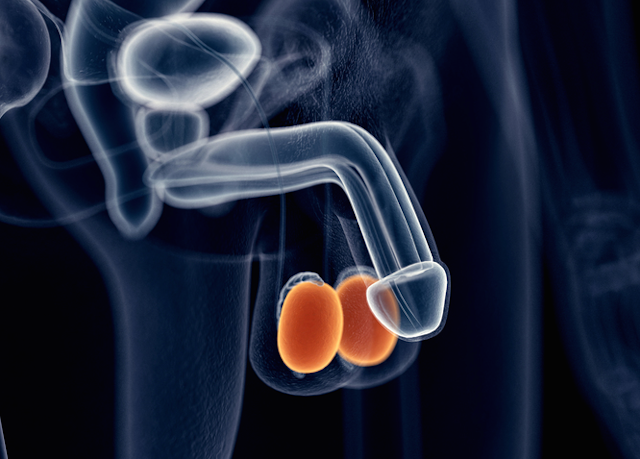
Klinefelter’s syndrome is not commonly diagnosed, with only four in 10 men diagnosed after birth and 10% diagnosed pre-puberty. Klinefelter’s syndrome is not typically diagnosed at birth, although physical characteristics may include a small penis and undescended testicles.
Klinefelter’s syndrome is the most common form of hypogonadism, where men are unable to produce sperm or sufficient levels of the male sex hormone, testosterone. The low levels of testosterone result in the underdevelopment of typical male characteristics.
Symptoms of Klinefelter’s syndrome vary between individuals, but typically include small testicles, lack of facial, pubic and underarm hair, gynaecomastia (breast tissue enlargement), poor muscle development, disproportionately long arms and legs (compared to the body), and potential learning and language difficulties.
As adults, men with Klinefelter’s syndrome are infertile, as the extra X chromosome affects the ability to produce sperm, known as azoospermia. Men with this condition may also experience a low libido, depression and are at risk of osteoporosis.
Causes
While Klinefelter’s syndrome is a genetic disorder, it is not one that is inherited, as brothers of men with Klinefelter’s syndrome typically have the 46XY pattern.
The addition of the extra X chromosome is believed to occur as a random event during the formation of the reproductive cells, either within the fertilised egg or during cell division as the baby develops.
Diagnosis
Klinefelter’s syndrome can be diagnosed through a variety of tests. Physical examination of the genitals will confirm the size of the testes, with the size typically less than four millilitres (the size of a sultana grape).
Klinefelter’s syndrome can be confirmed using a blood test, which involves chromosomal analysis. Further blood tests can also examine the levels of testosterone (and other sex hormones), as well as semen examination for levels of sperm. Klinefelter’s syndrome may also be diagnosed prenatally, through maternal blood testing.
Treatment
Men diagnosed with Klinefelter’s syndrome cannot be cured; rather treatment aims to overcome some aspects of the symptoms. Hormone therapy, specifically testosterone replacement, is a lifelong therapy that increases physical strength, body tone and general wellbeing in men.
Testosterone therapy is available in various formats including gels, injections, lotions, creams and patches. If diagnosis occurs during the teenage years, testosterone therapy is initiated at a low dose and increased through the adult years.
In some men with Klinefelter’s syndrome, sperm may be found in the testicular tissue. For such men, assisted reproductive therapies such as intracytoplasmic sperm injection (ICSI) may be used to achieve pregnancy with their partners. ICSI is a form of in vitro fertilisation (IVF) whereby a single sperm is injected into each egg during the IVF procedure.
Donor insemination and adoption are alternatives in cases where assisted reproductive therapies are not an option.
Cosmetic surgery may be performed to remove the enlarged breast tissue. Counselling, physical and speech therapy may also be performed to assist men with the psychosocial aspects of the diagnosis.
Why is it hidden?
Lack of knowledge, awareness and psychosocial impact are all reasons Klinefelter’s syndrome is typically underdiagnosed. Men typically use health services less frequently than women. Even when men do see a doctor, a reproductive health examination is not routinely performed.
Few men have ever heard of Klinefelter’s syndrome, and similarly would be unaware of the symptoms. For example, many men would not know what the typical size of the testes is, and so may be unaware they have small testes.
In teenagers, symptoms of Klinefelter’s syndrome may be clouded by learning problems and the onset of puberty, with Klinefelter’s syndrome not primary in the thoughts of many health professionals. Embarrassment, stoicism and fear of the unknown are common psychosocial issues perceived by men that prevent them from seeing their doctor about reproductive health issues.
Treatment and management strategies for Klinefelter’s syndrome can ensure men diagnosed with the condition have good health outcomes. Further engagement with Klinefelter’s syndrome support groups can provide men with peer support and assist in overcoming any perceived psychosocial barriers associated with its diagnosis.
Further reading:
Dads get postnatal depression too
Men more reluctant to go to the doctor - and it’s putting them at risk
Breast cancer campaigns might be pink, but men get it too
How’s your walnut, mate? Why men don’t like to talk about their enlarged prostate
Correction: the chromosomal arrangement has been corrected to say 47XXY