There has been a significant increase in the number of children with strep A infections in the UK over the past month compared with the same period in previous years. Sadly, nine children have died as a result of complications of this bacterial infection.
The UK Health Security Agency (UKHSA) has issued a statement about what parents can look out for as signs of illness, and an alert notifying doctors about the rise in cases.
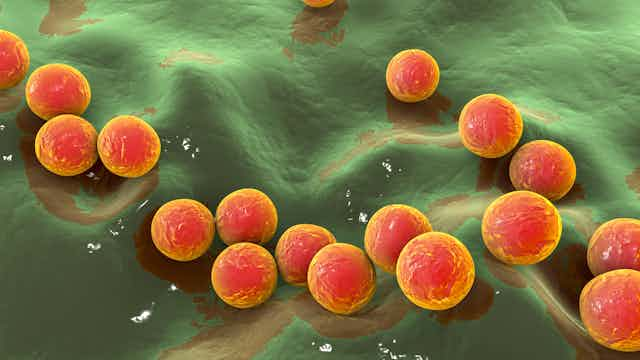
Group A streptococcus (also called GAS or strep A) is a type of bacteria that can live in the back of the throat or on the skin, especially in children. It can spread between people through close contact or coughing and sneezing.
In most people, it either causes no illness or only mild throat or skin infections or scarlet fever. Children with scarlet fever have a sandpaper-like rash over their body, often with fever and sore throat and a “strawberry tongue” - where the tongue is red with a white covering.
Read more: Scarlet fever outbreak in Scotland: what you need to know
While most rashes and sore throats in children are caused by viruses and so aren’t helped by antibiotics, these mild strep A bacterial infections can be easily treated with antibiotics. Taking antibiotics for strep A helps prevent any complications or spread to household and school contacts.
Children with scarlet fever should be kept at home until at least 24 hours after starting antibiotics to avoid passing on the infection.
Very rarely, strep A escapes from the skin or throat and causes a condition known as invasive group A strep, or iGAS. This leads to serious illness or even sepsis, including infections of the bloodstream, joints, bones, muscles, lungs, brain or deep skin layers (necrotising fasciitis). Children with invasive group A strep need to be treated in hospital with intravenous antibiotics.
Immunity debt
There has also been an increase in the usual winter respiratory viruses going around, with a particularly early and steep rise in cases of respiratory syncytial virus (RSV), a common childhood infection. During the pandemic lockdowns, fewer children were exposed to these viruses and therefore did not build up immunity to them, which has been termed “immunity debt”. Due to increased social mixing, many children are now picking up these viruses.

The increase in respiratory viruses this winter might be part of the reason behind the rise in cases of more serious invasive group A strep. The lining of the nose and throat becomes inflamed during viral illnesses, and this may allow the strep A bacteria to get into the bloodstream or the lungs.
Invasive group A strep is also more common in people with a weakened immune system, and people with skin sores or wounds, such as with chickenpox. These all help the bacteria get into deeper parts of the body, turning a mild infection into a serious one.
The rise in mild strep A infections may be due to increased social mixing and high amounts of circulating bacteria. Since a very small percentage of strep A infections lead to serious illness or invasive group A strep, it makes sense that the number of severe infections has risen as the overall numbers of mild and symptomless strep A infections have increased.
Public health and microbiology experts continuously analyse the circulating strains of strep A. The strains circulating in the UK at the moment are the same as those seen in recent years, so it is unlikely that a new or particularly aggressive strain is responsible for the increase in cases.
Very rare, but look out for this
While it is important to be aware of the increase in strep A infections, invasive group A strep is still thankfully very rare. Most people with strep A won’t develop invasive infection even if they have skin wounds or viral respiratory infections.
Signs to look out for are the same as for other serious illnesses in children:
- a high fever that is not settling in a child who seems unwell
- severe muscle aches
- pain in one area of the body
- a spreading redness on the skin (which may be harder to spot on darker skin)
- difficulty breathing
- excessive sleepiness or irritability.
Further information about when parents should be worried about their child can be found on the Healthier Together website.
Parents and carers are understandably likely to be feeling very anxious about strep A infections at the moment, but the risk for each child remains very small.
If too many children with mild infections attend the GP or emergency departments, it will make it harder for the very few children with severe disease to access care. The advice on the Healthier Together website will help parents to know when to seek medical attention.
Update: For signs of iGAS infection, we have added “(which may be harder to spot on darker skin)” for clarity.