When you think of tattoos you probably imagine bikies, celebrity tats or that Japanese flourish on your left foot that means “Honour” (or so you think).
You probably don’t picture medical revolution … which is what tattoos may now represent. Well, temporary tattoos, at least.
Work published today in Science shows how a simple stick-on tattoo could be used in a medical context.
Think of a patient in hospital overnight with a heart complaint. With existing technology, the patient might be hooked up to an electrocardiogram (ECG) device in order to monitor their heart.
Those devices use skin electrodes to pick up readings from the patient but unfortunately, there are significant drawbacks to using electrodes.
Worn for more than a few hours, they can start to leave marks, and on sensitive people (or when left on for longer than recommended) they can leave some impressive welts.
In the case of non-disposable electrodes, the application of conductive gel and cleaning (or even abrasion) of the skin is required.
The new development by Dae-Hyeong Kim and colleagues at the University of Illinois could put an end to the use of surface electrodes forever.
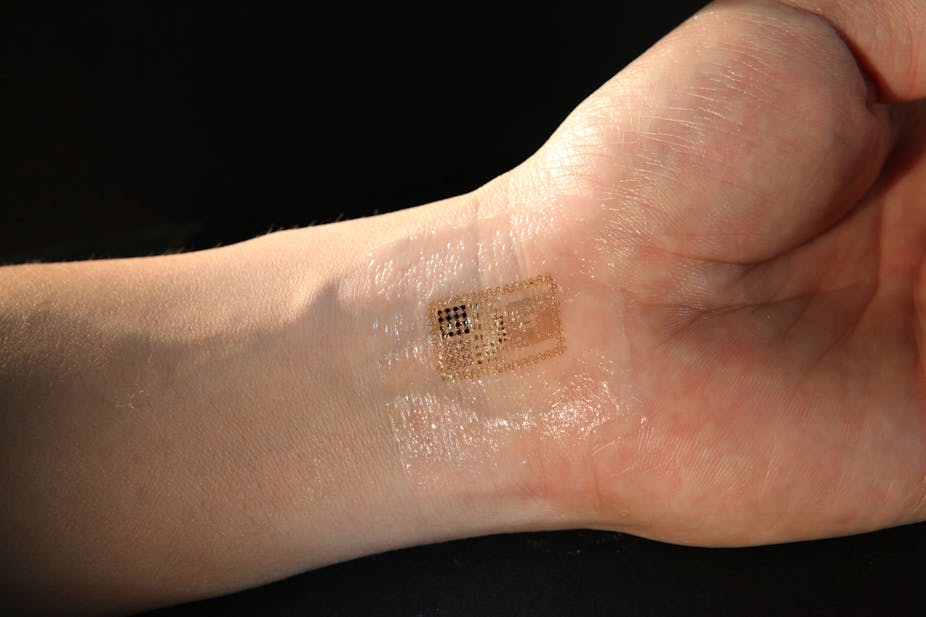
Using recent developments in nanotechnology, the team has developed a technique for printing electronic circuits on to water-soluble polymer sheets that can be applied like a “temporary tattoo”.
This development blurs the line between biology and electronics and offers nothing less than the possibility of completely unobtrusive, fully wearable, biological monitoring – with no electrodes in sight.
The researchers have dubbed it the “epidermal electronic system” (EES), and it has exciting possibilities in a range of disciplines:
In cardiac electrophysiology (i.e ECG):
Cardiology patients under observation over the course of a day typically wear a Holter heart monitor. Such devices are usually attached for a minimum of 24 hours (and often substantially longer) to capture the behaviour of the heart.
By making equipment lighter and wearable, it might be possible to continuously monitor patients who have known cardiac illnesses which put them at risk of heart attack.
A wearable “skin” sensor with an integrated circuit to detect arrhythmias – irregularities in the heart beat – could conceivably monitor individuals with a known cardiac problem or those who have a high-risk of developing such a condition – people with anorexia, for example.
In my field (heart rate variability), we extract measurements of the autonomic nervous system – the part of the nervous system that controls involuntary actions – from the beat-to-beat changes in the heart.
Comfortable, unobtrusive electrodes will allow us to monitor patients or experiment participants over very long periods of time, and investigate the very long-term changes in the variation of the heart.
Currently, we know almost nothing about what these changes represent.
In exercise physiology:
The firing rate and contraction force of the muscles are monitored by surface electrodes of an electromyogram (EMG).
These devices are quite bulky, and often prevent full, violent or natural movements to be studied while athletes are performing at their peak. (Try running at full speed while carrying an extra device and a dozen electrodes stuck to each leg!)
With a “skin” electrode it may be possible to monitor athletic performance completely without any noticeable difference from normal.
If the information can be accessed in real time, it may be possible to monitor the loss of force development over time during training itself and adjust accordingly – almost as if your muscles were “talking back to you” from under the skin.
In neurology:
One of the main problems with existing electroencephalogram (EEG) techniques – measuring the electrical activity of the brain using electrodes placed on the scalp – is the fact that participants are placed in artificial situations: stuck in a lab chair, barely able to move, watching stimuli on a screen.
But with the fully wearable, portable and invisible EES system Kim and colleagues have developed, we could monitor the same signals in real life, as they actually happen.
Moreover, in the case of conditions such as lateral temporal lobe epilepsy, it may be possible to pick up patterns indicative of seizures, directly from electrodes layered across the surface of the scalp.
All of this is just the beginning.

Kim and colleagues have already tested a number of these possibilities. Soon, instead of merely being passive sensors, the EES might entail whole integrated printed circuits that are able to measure biosignals, correct and analyse those signals, and provide feedback from digital devices in real time, all the time.
Psychophysiological experiments are frequently concerned with “external validity” – whether or not what we measure in the lab sufficiently represents the phenomena we’re trying to model in the real world.
With this system, that concern may soon be a thing of the past, as we won’t even be able to see the equipment.
So how long until we see this technology in Australian hospitals?
Well, if EES systems are classified as a medical device – and considering their role, that’s entirely likely – there will be some years of testing before they can be successfully employed in treatment.
It’s very hard to say when any device will be brought to market, but in around two years our laboratory will be asking suppliers if the EES is available for purchase yet.
Read more about the EES at our news story.